1. Empty your kettle and refill it with at least one litre of fresh tap water from the cold tap. Do not use water that has been previously boiled or water that has been softened. Bottled water is not recommended to make up a feed as it is not sterile and may contain too much salt (sodium) or sulphate.

2. Boil the water. Leave the water to cool in the kettle for no more than 30 minutes, so that it remains at a temperature of at least 70°C. If less water is used, the cooling time will be significantly shorter.

3. Clean and disinfect the work surface you are going to use. It is also really important that you wash your hands with soap and water to stop bacteria spreading.
4. If you are using a cold-water steriliser, shake off any excess sterilising solution from the bottle and the teat, or rinse the bottle with cooled boiled water from the kettle (not the tap).

5. Keep the teat and cap on the upturned lid of the steriliser. Avoid putting them on the work surface.
6. Follow the manufacturer’s instructions and pour the correct amount of water into the bottle first. Double check the water level is correct.

7. Loosely fill the supplied scoop with the formula powder and level it off using either the flat edge of a clean, dry knife or the leveller provided. Follow the manufacturer’s instructions and only put the suggested number of scoops in the bottle.

8. Holding the retaining ring, put it on the bottle and screw it on. Cover the teat with the cap and shake the bottle until the powder is dissolved.

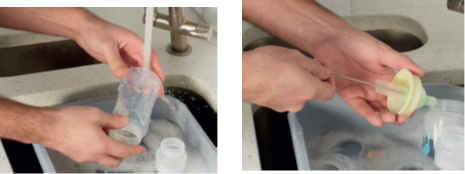
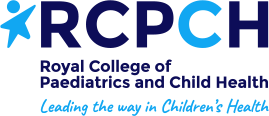
9. It is really important to cool the formula, so it is not too hot to drink. Cool the formula by holding the bottom half of the bottle under cold running water. Move the bottle about under the tap to ensure even cooling.

10. Test the temperature of the formula on the inside of your wrist before giving it to your baby. It should be body temperature, which means it should feel warm or cool, but not hot.
11. If there is any formula left in the bottle after a feed, throw it away.
12. To reduce the risk of infection, make up formula feeds as your baby needs them. One at a time.



 Feed your baby when they show signs of being hungry. Look for
Feed your baby when they show signs of being hungry. Look for  Hold your baby close in a semi-upright position, so you can see their face. Reassure them by looking into their eyes and talking to them. Begin the feed by gently rubbing the teat of the bottle against their top lip, inviting them to open their mouth.
Hold your baby close in a semi-upright position, so you can see their face. Reassure them by looking into their eyes and talking to them. Begin the feed by gently rubbing the teat of the bottle against their top lip, inviting them to open their mouth.  Gently insert the teat into your baby’s mouth, keeping the bottle in a horizontal position so that just enough milk covers the hole in the teat. This will stop the milk from flowing too fast.
Gently insert the teat into your baby’s mouth, keeping the bottle in a horizontal position so that just enough milk covers the hole in the teat. This will stop the milk from flowing too fast.  Your baby may need some short breaks during the feed and may need to occasionally burp. Watch your baby and follow their cues for when they need a break. Cues will vary from one baby to the next. They may splay their fingers and toes, spill milk out of their mouth, stop sucking, turn their head away or push the bottle away. When you see these cues, gently remove the teat from your baby’s mouth or tilt the bottle downwards to cut off the flow of milk. When your baby does not want any more milk, hold them upright and gently rub or pat their back to bring up any wind.
Your baby may need some short breaks during the feed and may need to occasionally burp. Watch your baby and follow their cues for when they need a break. Cues will vary from one baby to the next. They may splay their fingers and toes, spill milk out of their mouth, stop sucking, turn their head away or push the bottle away. When you see these cues, gently remove the teat from your baby’s mouth or tilt the bottle downwards to cut off the flow of milk. When your baby does not want any more milk, hold them upright and gently rub or pat their back to bring up any wind. 








 +
+  +
+  +
+  +
+ +
+ +
+ +
+ +
+  +
+ +
+ +
+ +
+ +
+ +
+