Fainting
Pregnant women can often feel faint. This is due to hormonal changes. Fainting happens if your brain is not getting enough blood and, therefore, not enough oxygen.
You are most likely to feel faint if you stand up too quickly from a chair or when getting out of a hot bath, but it can also happen when you are lying on your back.
Avoiding feeling faint
Here are some tips to help avoid feeling faint:
- try to get up slowly after sitting or lying down
- eat small regular meals and stay well hydrated by drinking plenty of water
- if you feel faint when standing still, find a seat quickly and the faintness should pass – if it doesn't, lie down on your side
- if you feel light headed while lying on your back, turn onto your side. (During pregnancy it is advisable to lay on your left side rather than your back)
It's better not to lie flat on your back in later pregnancy or during labour. The weight of your baby, uterus (womb), amniotic fluid and placenta can press on the main blood vessels that run down your back and can reduce the amount of blood returning to your heart.
Symptoms
You may experience the following symptoms just before fainting:
- yawning
- a sudden, clammy sweat
- feeling sick (nausea)
- fast, deep breathing
- confusion
- light headedness
- blurred vision or spots in front of your eyes
- ringing in your ears
This will usually be followed by a loss of strength and you then passing out.
When you collapse to the ground, your head and heart are on the same level. This means your heart doesn't have to work as hard to push blood up to your brain. You should return to consciousness after about 20 seconds. Fainting is not usually a cause for concern; however see below for advice about when you should seek advice.
For more information on local services please click here.
When should you get help?
When to call an ambulance:
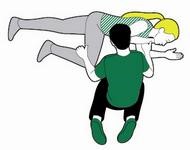
- If they have not come round after 1 minute or they do not come round. Call 999. Put them in the recovery position (see diagram). Ensure they are not lying on her back- where possible lay them on their left side.
- Signs of fits or jerking movements.
You need urgent help.
Go to the nearest Hospital Emergency (A&E) Department or phone 999
Call your maternity unit if you:
- Have fallen and landed on your tummy
- Have felt reduced baby movements since fainting
- Are taking medications for your blood pressure
- Have fallen and hit your head
You need to contact your maternity unit
Self care at home if you have no red or amber signs
- After fainting, it is normal to feel confused and weak for about 20-30 minutes. You may also feel tired and not be able to remember what you were doing just before you fainted. You may need to rest or ask someone to drive you home.
- Discuss this with your midwife at your next appointment
- Click here for more information
Self care
Contact your maternity unit if you are still concerned
Your local maternity unit is staffed 24 hours a day with
obstetrician s and midwives to help care for you, your baby and your pregnancy
related health concerns. For some AMBER
concerns it may be possible to be seen in a midwifery led unit if it is more
convenient for you. For health concerns that are not related to your pregnancy
you are advised to see your GP, call NHS 111 out of hours, or attend A&E if
it is an emergency.
To find the contact numbers for your local maternity unit, please click here.
- Labour line (maternity advice line) - Many maternity units provide women with a central advice line often called “labour line”. You are advised to call this number if you think you might be in labour. The phone is answered by a midwife 24hours a day. They will ask you questions, assess you and give advice. When the time is right they will arrange for you to attend your preferred place of birth, or arrange a midwife to come to you if you are planning a homebirth.
- Community Midwife- Your community midwife provides you with all routine maternity care from your first “booking in“ appointment in early pregnancy to discharging you to the care of the health visitors when your baby is 2 weeks old. She will give you information on keeping you and your baby healthy during pregnancy and refer you to specialists if required.
Whilst you may have individual contact details for your community midwife, if you are concerned about your pregnancy we advise you call the maternity unit on the numbers provided because staff are available 24 hours a day. Please do not leave urgent voicemails or text on a community midwife’s phone.
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and can arrange referral to a hospital specialist should you need it. Whilst pregnant, you will have regular appointments with a midwife but it is still important to continue with any ongoing care from your GP.
NHS 111 can ask you questions to assess your symptoms, give you advice or can put you in touch with a GP out of usual working hours.
A&E departments provide vital care for life threatening emergencies, such as suspected heart attack or breathing difficulties. If you are not sure it’s an emergency, call 111 for advice.